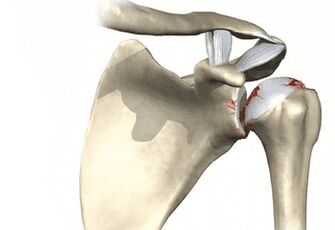
The shoulder joint is one of the most vulnerable joints in the human skeleton. This is due to the rather complex joint structure with weak fixation to the shoulder blade. The shoulder is subjected to a large amount of stress every day when performing household or professional tasks. If an injury occurs, metabolic processes are disrupted, tissues wear out with age - dystrophic changes in cartilage tissue begin. This disease is called shoulder osteoarthritis.
Depending on the manifestations and degree of damage to the glenohumeral joint, four degrees of pathology are diagnosed. There is also a difference between acute and chronic shoulder arthritis. If treatment is not performed promptly or in good faith, the joint will continue to deform and collapse, eventually leading to significant limitation of upper limb function and loss of mobility.
Currently, only grade 1 shoulder osteoarthritis can be completely cured. But this does not mean that you can give up and do nothing with grade 2 or higher pathology. Comprehensive and complete treatment of shoulder osteoarthritis with medication or surgery helps slow down the process of joint destruction, at least partially preserve the mobility of the arm and shoulder, and prevent disability.
Symptoms and causes
Shoulder deformity does not develop in a day. At first the changes were small. Cartilage gradually loses its elasticity under the influence of various factors - these can be age-related changes or disruptions in metabolic processes in the tissue. Small cracks appear on its surface, in which calcium salts accumulate. Then it becomes fragile, fragile and begins to collapse.
Often this process is accompanied by inflammation, which also spreads to surrounding muscle, connective and bone tissues. This manifests itself primarily as pain - at first mild soreness. They then become more intense and at an advanced stage never go away, which significantly reduces a person's performance and quality of life.
The main reasons why DOA of the shoulder joint develops are as follows:
- Blood circulation is impaired in the cartilage tissues of the shoulder in atherosclerosis and other chronic diseases related to blood vessels.
- Chronic diseases of an autoimmune nature, such as rheumatoid arthritis and systemic lupus erythematosus.
- Dysfunction of the endocrine system (diabetes mellitus).
- Congenital defects of the shoulder joint, birth trauma in infants and other injuries lead to pathological deformities and limb dysfunction.
- Acquired pathologies of joint structures after trauma or accident, unsuccessful surgery, including inflammation due to arthritis, synovitis, osteoporosis, etc. v.

In addition, there are provoking factors that increase the risk of shoulder arthritis many times over. Including:
- occupational activities in which the shoulder joint is subjected to heavy loads day after day for many years - shoulder arthritis is quite rightly called the disease of plasterers, painters and stevedores;
- sedentary lifestyle, lack of physical activity - insufficient exercise, blood circulation slows down, joint tissues do not receive the necessary amount of nutrients and begin to atrophy;
- overweight - often combined with the previous factor; with obesity, a person cannot move actively, while the joints are subjected to additional stress due to extra pounds;
- genetic predisposition;
- Old age - about 80% of people over 70 years old have symptoms of osteoarthritis.
Usually, when examining and interviewing the patient, the doctor determines a combination of several diseases and provoking factors. A typical patient diagnosed with shoulder osteoarthritis is a man or woman over 50 years old, does heavy work, is overweight, and has other chronic diseases (diabetes mellitus, hypertension, varicose veins, knee arthritis, etc. ). In this case, damage to the right shoulder is more common than the left shoulder. This is because most people actively use their right hand at work and at home, with the exception of naturally left-handed people.
How to recognize the disease
Symptoms of shoulder osteoarthritis may not appear for a long time. If from time to time the shoulder begins to hurt, a person believes that it is due to fatigue, takes painkillers, uses ointments that have a warming and calming effect. But sooner or later there will come a time when the drugs and ointments no longer work, the pain becomes constant, intense and makes you uncomfortable at rest and at night. In addition to this symptom, the following signs will indicate dystrophic changes in the shoulder joint:
- joint swelling and deformity, visible to the naked eye;
- redness of the skin on the joints, increased local temperature;
- characteristic clicking sound in the joints. The creaking sound when the hand moves vigorously is explained by the accumulation of salts in the cracks of the cartilage and between the parts of the joint. At first, the crunching sound occurs only when there is a sudden movement, it is quiet and almost inaudible. In the advanced form of the disease, the shoulder twitches with every movement, sounds are heard by others;
- Restriction of limb movement. When examining a patient, the doctor will ask the person to comb their hair. This test is enough to diagnose shoulder osteoarthritis: the patient will feel sharp pain, rotate the shoulder, the shoulder will be difficult to move back, the doctor will hear cracking and clicking sounds in the joint.

DOA of the shoulder must be treated, otherwise over time the patient will completely lose mobility and mobility of the upper limb. If the process of destruction of cartilage and surrounding tissue has begun, it will not stop on its own. Proper nutrition, folk remedies, healthy lifestyle and exercise are not enough here. To cope with the problem and prevent disability, complex treatment will be required using drugs of different effects and physical procedures.
Degree
There are several stages of shoulder DOA, each presenting differently and requiring a different treatment approach.
- Degree 1.At this stage, the disease has just begun to develop, changes in cartilage tissue are still small. The main symptoms of grade 1 DOA are joint and extremity weakness and periodic persistent pain. The pain occurs after exertion, when making monotonous, repetitive hand movements for a long time. After a night of sleep or long rest, a person feels stiffness in the shoulder joints, but as it develops, the stiffness still disappears without medication and physical procedures - a light warm-up is enough. If you take an X-ray at this stage, the images will not show significant changes in the joint structure, although thinning and deformation of the cartilage may be evident.
- Level 2 degree.The pathological process takes place and manifests itself more actively. A person is used to the fact that after work his shoulder will hurt, he "waits" for the pain, there are painkillers and ointments for joint pain, available at the pharmacy or homemade. X-ray diagnosis will show obvious changes in the joints: thinning and deformity of the cartilage, inflammation of the joint membrane. Occasionally, the joint turns red and swells, and when moving, crunching, creaking and rattling sounds can be heard.
- Level 3 degree.The shoulder joint hurts and makes a constant crunching sound. To reduce the discomfort, the patient tries not to touch it or move it at all. The deformation is visible to the naked eye; The affected shoulder is a different size and shape than the healthy shoulder; it often turns red and swollen, accompanied by increased pain. They cannot be removed with painkillers.

If nothing is done in the third stage of the disease, the fourth stage will occur - the shoulder joints and limbs are completely immobile. In this case, prescribing medication and physiotherapy is meaningless, only arthroscopic surgery will help restore at least partial function of the hand. But even this is not always successful.
On a note:In medical practice, cases of grade 3 shoulder arthritis are extremely rare. Usually, patients seek medical help earlier and begin treatment. Severe cartilage destruction can occur as a result of severe trauma, if for some reason the patient cannot see a doctor, or if the person lives in difficult social conditions where there are no qualified doctors.
How is arthritis diagnosed and treated?
A good doctor will be able to make a preliminary diagnosis after a conversation with the patient and an external examination. More specific diagnostic methods are needed to exclude other pathologies and complications or to identify them. To accurately determine the severity of the affected joint and whether inflammation has occurred, the following diagnostic measures are performed:
- X-ray;
- CT scan;
- Magnetic resonance imaging;
- in some cases, ultrasound to get a full picture of the condition of the joint;
- Clinical urine and blood tests - white blood cell count and erythrocyte sedimentation rate will be assessed. If they are too high, an inflammatory process will develop in the body.
The best way to treat pathology is determined by the doctor on an individual basis, taking into account the patient's age, occupation and general condition.
Traditional treatment involves the use of the following methods and means:
- A course of treatment with non-steroidal anti-inflammatory drugs. The drug is prescribed in the form of tablets or powder for oral administration or in the form of ointments for external use to eliminate the main symptoms of inflammation - pain, swelling, redness, increased body temperature.
- Anesthesia for severe pain comes in tablet or injection form. These drugs cannot be taken continuously, they do not eliminate the cause of the disease and are intended only for severe cases when the pain is unbearable.
- A course of chondroprotectors - drugs that promote the recovery of cartilage tissue and prevent further destruction. They also partially reduce pain, swelling and deformity of the shoulder joint. These drugs do not work immediately but need to be used for at least 3-4 months.
- A course of muscle relaxants - pills or injections that help relax muscle spasms. These are optional drugs in the complex treatment of osteoarthritis and are not always prescribed.
- A course of using vitamin-mineral complexes and dietary supplements with collagen and hyaluronic acid.

To increase the effectiveness of treatment, speed up recovery and prevent new damage, a special therapeutic nutritional regimen is also prescribed. The patient's diet includes foods rich in vitamins B, A, C, E - fresh fruits and vegetables, cabbage of all kinds, cereals, legumes. Polyunsaturated fatty acids can be obtained from marine fish and seafood. The gelatin diet is followed because gelatin helps restore the elasticity of cartilage tissue. The menu includes jelly meat made from ox hoof and tail, aspic and many different types of jelly. It is useful to use gelatin in its pure form, previously soaked in warm water.
Physical therapy is the next important point in the complex treatment of shoulder osteoarthritis. They are started only when the inflammatory process stops. Depending on the severity of the disease, progression and effectiveness of drug treatment, doctors choose a combination of the following physical methods:
- cryotherapy;
- Acupuncture;
- electrophoresis;
- laser therapy;
- magnetic therapy;
- mud therapy;
- massage of all kinds;
- physical therapy.
Physiotherapeutic procedures are aimed at activating metabolic processes in joint tissues, normalizing blood circulation and restoring limb mobility. With their help, it is possible to reduce the number of drugs taken and their dosage, which is especially valuable if the pathology is observed in teenagers, the elderly or lactating women.
Helpful advice:Grade 1-2 shoulder joint damage can be treated at home by using folk remedies. The main thing is that the patient does not forget to take the medicine on time and does not skip physical procedures - the effect will be noticeable and last only if all the doctor's prescriptions are regularly and conscientiously followed.

If conservative treatment is not effective, the doctor is forced to operate on the patient. The remainder of the destroyed joint will be removed and a prosthesis will be implanted in its place. Such interventions are not uncommon but require highly qualified doctors, precision and attention at every stage. In addition, the prosthesis does not always take root well, and the recovery period after surgery lasts at least six months. Therefore, if you notice that your shoulder begins to often hurt, pull, numb or hear a crunching sound when moving, do not delay in seeing a doctor, see a doctor promptly and, if necessary, takestart treatment.
Shoulder osteoarthritis is a fairly common disease of the musculoskeletal system, occurring mainly in people over 50 years old. The pathology develops gradually, little by little, under the influence of adverse factors, the joint structures begin to collapse, manifested by pain, swelling, and stiffness. In the early stages, the progression of the disease can be stopped with comprehensive treatment methods: medications, vitamin supplements, dietary therapy and physical therapy. Progressive osteoarthritis can only be treated with surgery.































